Wednesday, March 17, 2021
Is This Inhaler Effective for Respiratory Viruses?
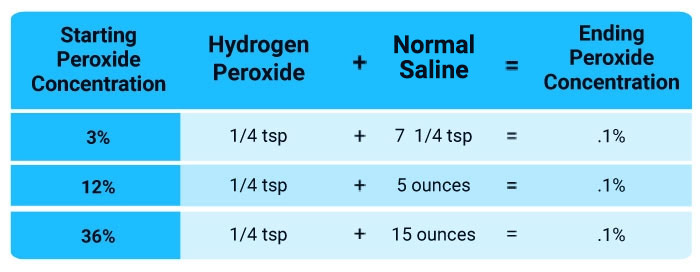
Please understand I am only posting information to be complete as this is NOT in any way, shape or form my primary recommendation for the treatment of COVID-19. There is little to no doubt in my mind that the most effective and safest treatment for this illness is nebulized diluted hydrogen peroxide at .1% with one drop of either 5% Lugol’s iodine or 2 drops of the 2% concentration.
Dr. David Brownstein has successfully treated more than 230 COVID-19 patients using immune boosting strategies such as intravenous or nebulized hydrogen peroxide, iodine, oral vitamins A, C and D, and intramuscular ozone. None has died from the infection.
I've embraced nebulized peroxide since the COVID-19 pandemic broke out and have received many anecdotal reports from people who have successfully used it, even at more advanced stages.
Based on Brownstein’s experience, I now also recommend adding iodine when nebulizing, as it appears to make it even more effective. You can find the details of using nebulized peroxide for COVID-19 by watching my interview with Brownstein below. The video embedded in our interview is a more detailed explanation of hydrogen peroxide nebulization and how to do it.
Inhaled Steroid Treatments
During the early days of the COVID-19 pandemic, reports from China, Italy and the U.S. revealed something curious about patients hospitalized with COVID-19: Those with chronic respiratory diseases like asthma and chronic obstructive pulmonary disease were significantly underrepresented, according to a team of researchers from the University of Oxford.1
The team suggested this may be due to their widespread use of inhaled glucocorticoids, such as budesonide. Further, the onset of COVID-19 is typically mild, “giving a potential window to intervene prior to the development of severe disease,” they wrote in the preprint journal medRxiv. However, most studies have only focused on treating severe COVID-19 in hospitalized patients.
“There have been important breakthroughs in hospitalized COVID-19 patients, but equally important is treating early disease to prevent clinical deterioration and the need for urgent care and hospitalization, especially to the billions of people worldwide who have limited access to hospital care,” study author professor Mona Bafadhel said in a news release.2
The researchers conducted a randomized trial involving 146 people in order to determine if budesonide, when used early during COVID-19 infection, would improve outcomes, with promising results.
Early Inhaler Use for COVID-19
Of the 146 people in the study, half took 800 micrograms of budesonide twice a day within seven days of the onset of COVID-19 symptoms while half received usual care.3,4 Inhaled budesonide lowered the relative risk of needing urgent care or hospitalization by 90% over 28 days, while also resolving fever and other symptoms faster and leading to fewer persistent symptoms during the study period.5
Specifically, those taking budesonide recovered one day sooner than those who didn’t; clinical recovery occurred after a median of seven days in the inhaler group compared to eight days among those receiving usual care.6 Persistent symptoms were lower in the inhaler group at both 14 and 28 days compared to the usual care group. Bafadhel noted:7
“Although not the primary outcome of study, this is an important finding. I am encouraged to see the reduction in persistent symptoms at 14 and 28 days after treatment with budesonide. Persistent symptoms after the initial COVID-19 illness have emerged as a long-term problem. Any intervention which could address this would be a major step forward.”
The researchers also calculated the number needed to treat, or NNT, which describes how many people have to take a particular drug to avoid one incidence of a medical issue. In this case, the NNT with inhaled budesonide to reduce COVID-19 deterioration was eight.8
For comparison, influenza vaccines have an NNT, or NNV (number needed to vaccinate) of 71,9 meaning 71 people must be vaccinated to prevent a single case of confirmed influenza. Vitamin D has an NNT of 33 in terms of preventing acute respiratory tract infections,10 although among those who were severely vitamin D deficient at baseline, taking vitamin D had an NNT of four.
The researchers concluded, “Early administration of inhaled budesonide reduced the likelihood of needing urgent medical care and reduced time to recovery following early COVID-19 infection.”11
Inhaler Treatment ‘Equivalent’ to COVID Vaccine Effectiveness
According to the University of Oxford team, the main reason why people with asthma and COPD use inhaled glucocorticoids is to reduce exacerbations in their conditions, which are often caused by viral infections.
Studies in-vitro have previously shown that such inhalers reduce the replication of SARS-CoV-2, the virus that causes COVID-19, in airway epithelial cells.12 Airway epithelial cells act as the second line of defense after the mucus layer, acting as a physical barrier within your respiratory tract.
Inhaled glucocorticoids may also downregulate the expression of angiotensin converting enzyme-2 (ACE2) and transmembrane protease serine 2 (TMPRSS2), which play a role in the entrance of viruses into cells.13
A combination of drugs including budesonide has also been shown to inhibit the replication of coronavirus 229E, one cause of the common cold, by inhibiting receptor expression and may also help to modulate inflammation in the airways caused by the infection.14
The researchers noted that the 90% relative reduction in clinical deterioration seen after short-term use of budesonide is equivalent to the effectiveness of COVID-19 vaccines and greater than the effectiveness of any treatments currently used to treat hospitalized severely ill COVID-19 patients.
Further, in the event that mutated strains of SARS-CoV-2 become widespread, budesonide may have a notable advantage over vaccination, with researchers stating, “Unlike with vaccines, the efficacy of inhaled budesonide is unlikely to be affected by any emergent SARS-CoV-2 variant.”15
While there are some concerns about systemic effects of inhaled glucocorticoids when used long term, short-term use of the medications for purposes of treating COVID-19 may represent a relatively safe, low-cost and widely available intervention. According to the study:16
“The number of participants needed to treat to prevent increased health care resource utilization is 8, and combined with the short treatment period required to achieve benefit, makes this potentially an affordable and scalable intervention for early COVID-19.
This is especially significant in low- and middle-income countries where the majority of currently approved COVID-19 treatments are unlikely to ever reach patients as a consequence of variable healthcare systems.”
N-acetylcysteine (NAC) and Glutathione
A number of other treatments have also shown promise for the treatment of COVID-19. N-acetylcysteine (NAC) and glutathione are among them. NAC is a form of the amino acid cysteine.
It is most well-known to help increase glutathione and reduce the acetaldehyde toxicity17 that causes many hangover symptoms. Anyone who overdoses on Tylenol also receives large doses of NAC in the emergency room, as it helps prevent liver damage by increasing glutathione.
The reason why NAC and glutathione are valued for COVID-19 is because of the role they play in combating oxidative stress, which is a main cause of inflammation and disease in general, and the cytokine storm associated with COVID-19 in particular. NAC may also combat the abnormal blood clotting seen in many cases.
Research has demonstrated that NAC can attenuate symptoms of influenza and improve cell-mediated immunity. In terms of influenza, according to pulmonologist Dr. Roger Seheult in a MedCram lecture,18 NAC has an NNT of 0.5, which means for every two people treated with NAC, one will be protected against symptomatic influenza.19
Additional Treatments for Respiratory Viruses
Many options exist for COVID-19 treatments, although not many of them are being widely publicized. Following is a sampling of some of the options being considered:
• Vitamin D — Research published in November 2020 in the Postgraduate Medical Journal, shows oral vitamin D supplementation also helps speed up SARS-CoV-2 viral clearance.20 More than 200 doctors, scientists and leading authorities have signed an open letter calling for increased use of vitamin D in the fight against COVID-19.21
• Vitamin C — While health authorities and mainstream media have ignored, if not outright opposed, the use of vitamin C and other supplements in the treatment of COVID-19, citing lack of clinical evidence, a landmark review recommends the use of vitamin C as an adjunctive therapy for respiratory infections, sepsis and COVID-19.22
The review detailed vitamin C's mechanisms of action and how it helps in cases of infectious disease, including the common cold, pneumonia, sepsis and COVID-19. For starters, vitamin C has the following basic properties:23
- Anti-inflammatory
- Immunomodulatory
- Antioxidant
- Antithrombotic
- Antiviral
While high-dose vitamin C regimens typically call for intravenous administration, if treating a viral infection at home (be it COVID-19 or something else), you could use oral liposomal vitamin C, as this allows you to take far higher doses without causing loose stools.
You can take up to 100 grams of liposomal vitamin C without problems and get really high blood levels, equivalent to or higher than intravenous vitamin C. I view that as an acute treatment, however. I discourage people from taking mega doses of vitamin C on a regular basis if they're not actually sick, because it is essentially a drug — or at least it works like one.
• Hydroxychloroquine (HCQ) — HCQ, a so-called zinc ionophore and antimalaria, drug, has shown effectiveness against COVID-19. As early as March 2020, Dr. Vladimir Zelenko boasted a near-100% success rate treating COVID-19 patients with hydroxychloroquine (HCQ), azithromycin and zinc sulfate for five days.24 As of February 2021, Zelenko has treated 3,000 patients with COVID-19 symptoms and only three high-risk patients have died.
HCQ should be available to most people in the U.S. at this point, but you do need a prescription, and some doctors are still unwilling or resistant to prescribe it. If you can’t find HCQ, the nutritional supplement quercetin may be a useful (and perhaps even better) substitute, as its primary mechanism of action is identical to that of the drug. It also has antiviral activity of its own.
• Ivermectin — In December 2020, the Frontline COVID-19 Critical Care Alliance (FLCCC) called for widespread adoption of ivermectin, both as a prophylactic and for the treatment of all phases of COVID-19.25,26 In one trial, 58 volunteers took 12 milligrams of ivermectin once per month for four months.
Only four (6.96%) came down with mild COVID-19 symptoms during the May through August 2020 trial period. In comparison, 44 of 60 health care workers (73.3%) who had declined the medication were diagnosed with COVID-19.27
Early Treatment May Be Key
A common thread with many available treatments is that the earlier treatment starts, the better the outcomes tend to be. In the case of budesonide, for instance, treatment occurred within seven days of the onset of symptoms. In addition to early care, prevention is an even better option, and this is where strategies like vitamin D optimization become essential.
If you review my recent interviews with Drs. Brownstein and Zelenko you will learn that they have been in the trenches treating many with this illness and it has been their consistent observation that if this illness is treated early in the course of the disease you can virtually eliminate the risk of long term complications. So, the key is to treat early.
from Articles https://ift.tt/3vwVmgU
via IFTTT
No comments :
Post a Comment